Frontotemporal Dementia (FTD)
When Personality, Language, and Behavior Lead Decline
Overview
Frontotemporal Dementia (FTD) is a progressive neurodegenerative condition that primarily affects the frontal and temporal lobes of the brain. This leads to early and prominent changes in behavior, personality, and language, often before memory is noticeably impaired. Unlike Alzheimer’s, FTD emphasizes identity and social expression changes as core clinical features.
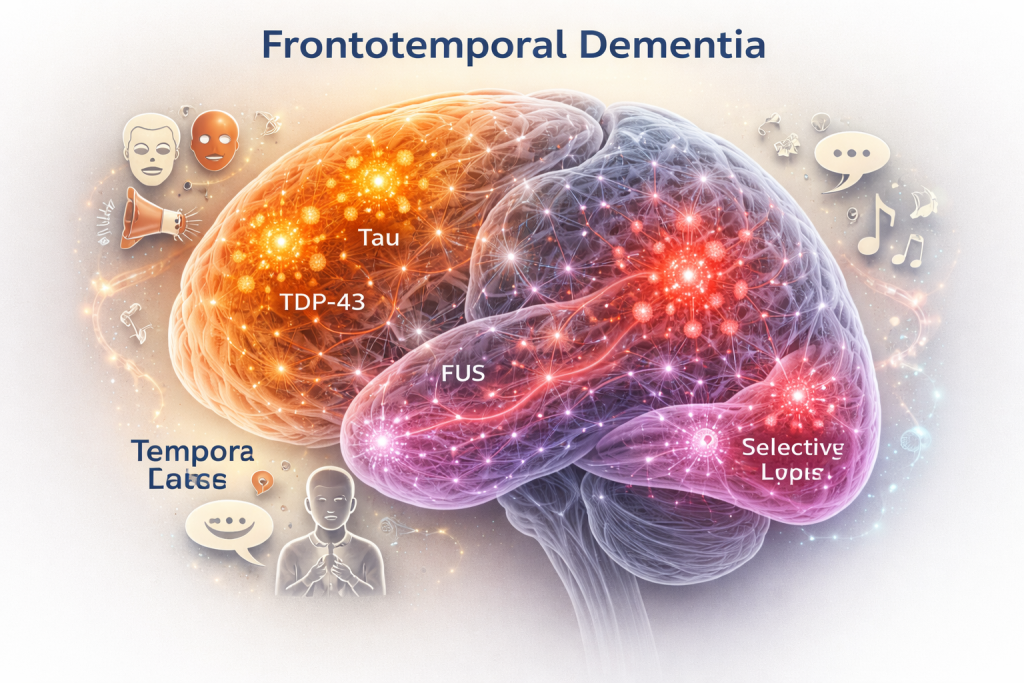
Pathological protein accumulations—including tau, TDP-43, and FUS—dictate the symptom patterns, creating subtle differences between cases while following characteristic network degeneration paths.
Primary System Failures
Selective Network Vulnerability
Specific frontal and temporal networks are more susceptible to degeneration, explaining why memory may remain intact while personality, decision-making, and social cognition deteriorate.
Proteinopathy-Specific Patterns
Tau, TDP-43, and FUS proteins drive unique symptom clusters. Early behavioral, language, and motor presentations are influenced by which protein is predominant.
Social Cognition Breakdown
Impairments in empathy, judgment, and adherence to social norms often precede measurable cognitive deficits, highlighting the lobar specificity of degeneration.
Overlooked Mechanisms
- Behavioral and language alterations can appear years before clinical diagnosis.
- Selective collapse of neural networks explains preserved memory despite personality changes.
- Subtle social cognition deficits are frequently misattributed to psychiatric or environmental factors.
- Progression is influenced by protein-specific pathogenic pathways, inflammatory responses, and network connectivity loss.
Action Orientation
Early recognition of behavioral and language changes is critical. Interventions may include:
- Supporting social and occupational engagement.
- Monitoring proteinopathy-specific risk factors.
- Implementing cognitive and behavioral therapies tailored to symptom clusters.
- Providing caregiver education and structured support environments.