Lewy Body Dementia (LBD)
Lewy Body Dementia (LBD) is a progressive neurodegenerative disorder characterized by abnormal intracellular protein deposits known as Lewy bodies. It is the second most common degenerative dementia after Alzheimer’s disease and presents a distinct overlap of cognitive impairment, Parkinsonian motor features, and neuropsychiatric symptoms. LBD is frequently underrecognized due to its clinical similarity to both Alzheimer’s and Parkinson’s disease.
Medical Word Breakdown: Lewy Body
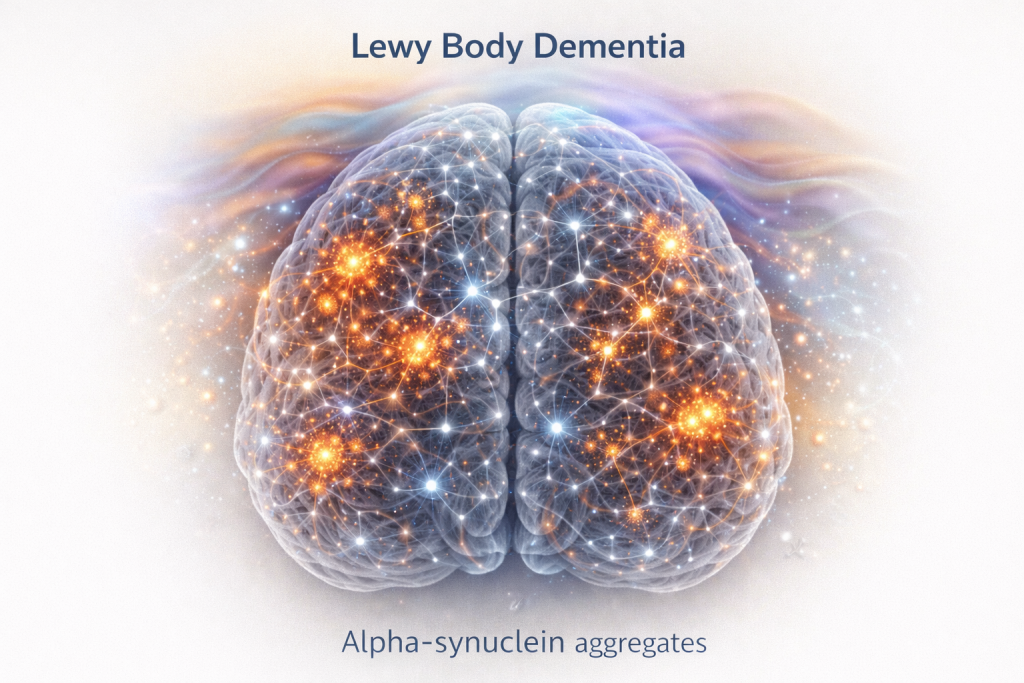
A Lewy body is an abnormal intracellular inclusion composed primarily of misfolded alpha-synuclein protein. These aggregates disrupt neuronal signaling, intracellular transport, and cellular survival mechanisms.
Core Biological Mechanisms
The pathological hallmark of LBD is widespread accumulation of alpha-synuclein across cortical and subcortical brain regions. Unlike Parkinson’s disease, where pathology often begins in the brainstem, LBD demonstrates early cortical involvement, accounting for its prominent cognitive and psychiatric manifestations.
- Diffuse cortical alpha-synuclein deposition
- Degeneration of cholinergic pathways
- Dopaminergic system impairment
- Progressive synaptic dysfunction and neuronal loss
Medical Word Breakdown: Alpha-Synuclein
Alpha-synuclein is a presynaptic neuronal protein involved in synaptic vesicle regulation. When misfolded, it forms toxic aggregates that impair mitochondrial function, protein clearance, and neuronal communication.
Clinical Presentation
Lewy Body Dementia is clinically defined by a characteristic triad:
- Cognitive fluctuations — marked variability in attention and alertness
- Recurrent visual hallucinations — vivid and well-formed
- Parkinsonism — rigidity, bradykinesia, postural instability
Additional non-motor features include REM sleep behavior disorder, autonomic dysfunction, mood disturbance, and anxiety. Memory impairment is often less pronounced in early stages compared to Alzheimer’s disease.
Medical Word Breakdown: Cognitive Fluctuations
Cognitive fluctuations refer to spontaneous and pronounced changes in cognition, alertness, and attention occurring over hours or days — a defining clinical feature of LBD.
Diagnostic Considerations
Diagnosis remains primarily clinical and is supported by targeted investigations:
- Dopamine transporter imaging (DaTscan)
- Polysomnography confirming REM sleep behavior disorder
- Cardiac MIBG scintigraphy demonstrating autonomic denervation
Structural MRI typically shows relative preservation of hippocampal volume compared to Alzheimer’s disease, particularly in early stages.
Pharmacological Management
Pharmacologic treatment requires caution due to medication sensitivity:
- Cholinesterase inhibitors (e.g., rivastigmine) for cognition and hallucinations
- Levodopa for limited motor symptom relief
- Dopamine-blocking antipsychotics should generally be avoided
Medical Word Breakdown: Neuroleptic Sensitivity
Neuroleptic sensitivity describes severe adverse reactions to dopamine-blocking antipsychotic medications, a well-documented risk in Lewy Body Dementia.
Non-Pharmacological Interventions
- Physical and occupational therapy for mobility and fall prevention
- Sleep optimization and REM disorder management
- Environmental simplification to reduce hallucinations
- Structured caregiver education and support
Prognosis & Outlook
Lewy Body Dementia follows a progressive but heterogeneous course. Early recognition and tailored management significantly improve safety, symptom control, and quality of life. Ongoing research focuses on alpha-synuclein biomarkers and disease-modifying strategies.